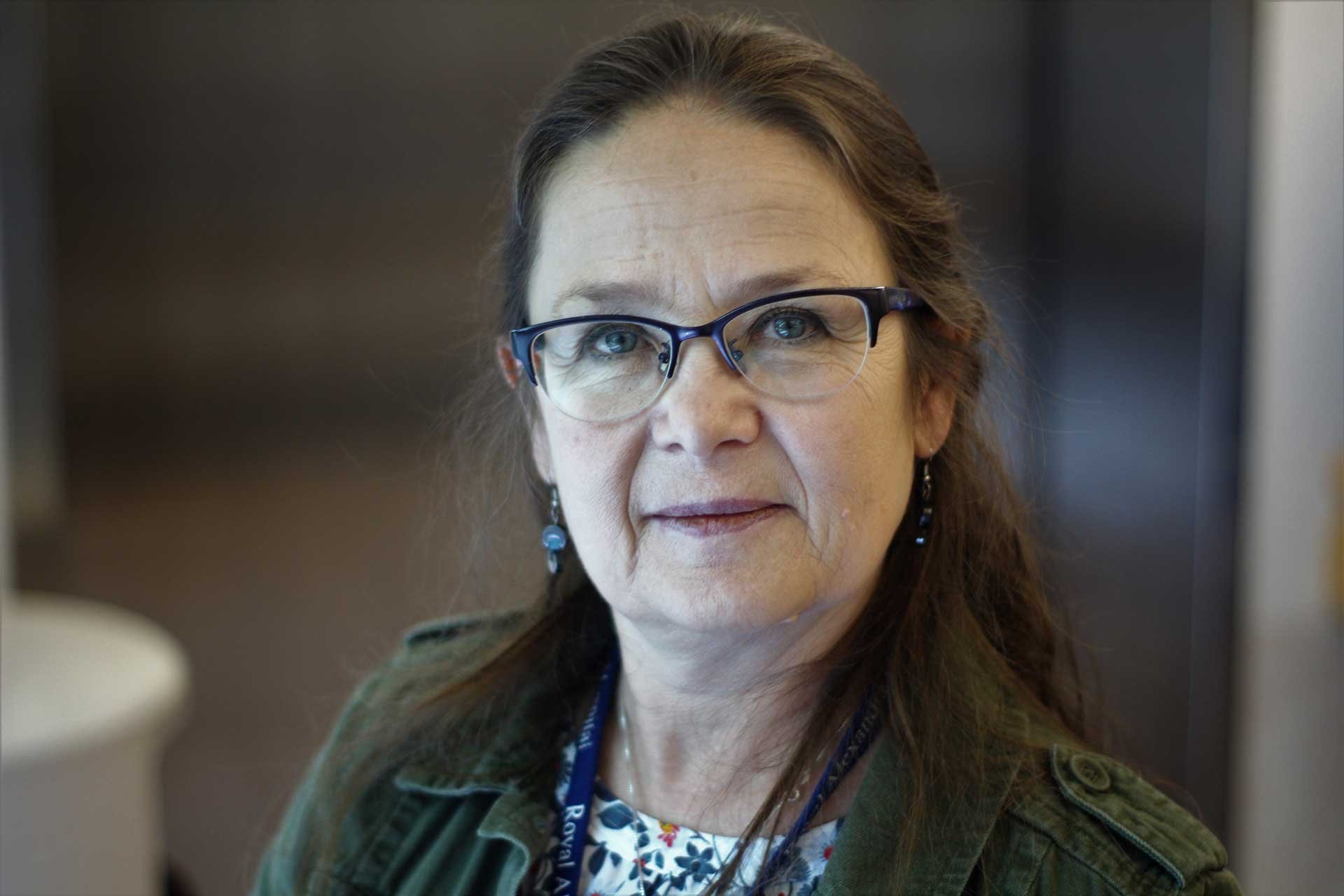
NP Teddie Tanguay: Making a Difference in the ICU
An intensive care unit (ICU) can be a scary place for patients.
For one thing you must be really, really sick to be there. You are hooked up to tubes, IV lines, and monitors. You hear distressed cries from patients and families, the beeps and buzzers, and the occasional “code blue” amplified over speakers.
Not only scary, but overwhelming. And not only for patients, but their families too.
Fortunately, at the Royal Alexandra Hospital ICU in Edmonton there is one constant presence that patients and families can turn to for support – the nurse practitioner.
Making a Difference
Teddie Tanguay, a past president of the Nurse Practitioner Association of Alberta, has worked in the ICU for most of her career, and as a nurse practitioner for the past 16 years. She is one of a team of nurse practitioners working on the unit. She uses her advanced nursing education to look at a health situation from both a medical and a nursing point of view and to develop treatment plans accordingly.
Tanguay’s practice is guided by “How do I make this journey better for patients and their families, during some of the worst moments of their lives?”
For one, Tanguay, along with the other NPs, is an almost constant presence in the ICU (whereas RNs and physicians are on rotations). She is available to patients and families – answering questions, providing status updates, and assisting with case management. She explains what families can expect from the ICU team, and she asks them how the team can give them support. “We really talk to families about the tests, the outcomes and the plan of care,” she says. “We include them in the hard discussions about their loved one. We try to make it very collaborative – to understand what their loved one would want.”
“My reward is working with patients and families and making a difference. This gets me out of bed every morning.”
While an ICU is a high stress environment, the adrenaline of working with the sickest patients, the continual learning, and the relationships she forges with patients, families and colleagues are what keep her working there.
Tanguay notes that the ICU is unique in that it is truly team-based – planning and priorities for care are established by all team members, including physicians, nurse practitioners, registered nurses, pharmacists, therapists and, as importantly, families.
“The team approach is real – it’s not just lip service; it’s how we practice.” And, in a very real way, the patient and family are part of the team.
The Role of ARNET
The Alberta Registered Nurses Educational Trust (ARNET) has supported Tanguay’s s practice over the years by providing funding for her to attend conferences.
“Right now, there is not a lot of employer funding support for nursing education. Nurses, especially non-union, look to ARNET for help. The conferences in the United States and Canada give us a chance to hear about the newest evidence, and what works in other critical care units,” she says. “We can then get ideas to improve care for our patients and families.”
She notes that without ARNET funding, many nurses would rely on short, local courses to meet their continuing education requirements. And, while valuable, they tend to focus on a more local “in-house” approach to care. The ability to go to intensive conferences in other locations exposes them to other approaches and innovations they can take back to Alberta.